Vitamin D: Metabolism and Physiology
Vitamin D is the only fat soluble vitamin which executes its biological action once its pro-vitamin form goes through series of modification via its exposure to solar UV-B. It prominently exist in two forms: cholecalciferol (vitamin D2) and ergocalciferol (Vitamin D3). Salmon, a fatty fish and animal products are main source of vitamin D3 and vitamin D2 is mainly derived from plant source like mushrooms. Pre-vitamin D3 is obtained through cutaneous conversion once it is exposed to sunlight from 7-dehydrocholesterol. Subsequently, pre-vitamin D3 reaches liver through vitamin D binding protein (VDB) and converted in to 25-hydroxyviatmin D (25OHD) by vitamin 25-hydroxylase (CYP2R1). But this form is still biologically inactive, kidneys have primary role in converting 25OHD to 1, 25-hydroxyvitaminD [1, 25(OH)2 D] mediated by (Cytochrome P450 Family) CYP27B1 presents in megalin, a endocytic receptor in proximal tubules. Since, renal epithelia is involved in this important conversion it can be logically interpreted that any perturbation in the morphology of renal cells will compromise vitamin D generation. CYP27B1 expression is regulated by parathyroid hormone (PTH), hypocalcemia, hypophosphatemia and calcitonin. In addition, 1, 25(OH)2D and fibroblast growth factor-23 (FGF-23) attenuate the level of CYP27B1, which subsequently decrease 1, 25(OH)2D levels. Vitamin D work as a fat soluble steroid hormone via binding to vitamin D receptor (VDR) which are expressed in various organs, such as heart, liver, blood vessel. Thus subjecting patients with cardiovascular and gastrointestinal disorders more towards vitamin D deficiency. However, 1, 25(OH)2 D has very limited half-life, its levels are not usually considered as an optimal marker for vitamin D level. However, 25OHD is 500 to 1000 times more stable than 1, 25(OH)2 D. Therefore, 25OHD is used by clinicians as a perfect marker for vitamin D insufficiency.
In general, 30-50% of the world population is known to have vitamin D deficiency, which roughly compromise 1 billion people. The optimal range for 25OHD is 25-80 ng/ml, whereas less than 10ng/ml levels are labelled as severe deficient individual. The food and Nutrition Board of the Institute of Medicine (IOM) have recently suggested Dietary Reference Intake (DRI) for individual aged between 9-70 years around 600IU/day. But few researchers disagree with this notion as according to them serum 25OHD levels should be 40 ng/ml and dosage of vitamin D should be optimized according to above mentioned value which can go up-to 1000IU/day.
Hypovitaminosis and Type 1 Diabetes
Hypovitaminosis and diabetes share a common trait that they both are pandemic. The international Diabetes Federation estimated that 285 million people are diabetic which is 7% of the total world population. In future this number is going to increase to 435 million by 2030.
We know that the type 1 DM (Diabetes Mellitus) is an immunomodulatory disorder in which unknown reasons trigger pancreatic islet beta cells destruction, and thus cause absolute insulin deficiency. Vitamin D deficiency has been associated with many immunomodulatory disorders like multiple sclerosis, inflammatory bowel disease, rheumatoid arthritis, and systemic lupus erythematosus to name few. Vitamin D is known to be an inhibitor of lymphocyte proliferation and thus suppresses immune response, in addition VDRs are expressed in T and B lymphocytes, thus vitamin D thought to modulate cytokine profile. To affirm our notion of hypo-vitaminosis and diabetes manifestation, non-obese diabetic (NOD) mice showed severity of diabetes with vitamin D deficiency. However, vitamin D supplementation significantly reduced the development of type 1 diabetes. Vitamin D also attenuate the cytokine induced expression Fas, which further regulate the proliferation of human islet cells.
Vitamin D deficiency and prognosis of type 1 diabetes has been inversely related in human population. Insufficient levels of vitamin D has been corroborated with increased possibility of type 1 diabetes in infants, studies conducted in North Europe with neonates showed decreased probability for onset of type 1 diabetes. Few studies also suggested the impact of vitamin D on restoring beta cell function in type 1 diabetes. Apparently, two studies suggested no impact on beta cell functioning with vitamin D administration. One study suggested that alfacaicidol restored beta cell functioning in children with type 1 diabetes. Cholecalciferol (2000IU/day) supplemented for 18 months showed lower inflammation and restoration of beta cell function without any change in glycaemia. Considering the promising outcome of above mentioned data, it can be said that vitamin D does have role in limiting the pathogenesis of type 1 diabetes, but still we need large and more organized trials for precise evaluation of vitamin D supplementation.
Vitamin D plays Important Role in Insulin secretion and it’s Sensitivity
Investigation conducted on rat pancreatic cell have shown that insufficient level of vitamin D severely impairs insulin secretion, as its supplementation restore normal secretory function of beta cells. As we have discussed above that VDR are present in various organs including pancreatic beta cells, thus vitamin D level can directly impact beta-cell functioning (Figure 1). Conditionally knockout mice lacking functional VDR have shown defective insulin secretion following glucose administration. It seems that vitamin D impact insulin synthesis which in turn perturb the amount of stored insulin. Beside this, vitamin D execute pivotal role in insulin synthesis and storage, it play additional role in maintaining calcium concentration and flux. Insulin secretion is dependent on internal and external calcium level. In addition, vitamin D regulates calbining a calcium binding protein involved in the release of insulin while maintain calcium homeostasis.
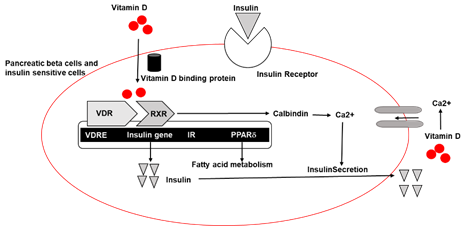
Vitamin D response elements are found in insulin receptor promoter, where VDR-retinoic acid X-receptor (RXR) complex binds with vitamin D and promotes the expression of insulin receptor without altering its affinity for insulin. Interestingly, vitamin D enhance fatty acid metabolism and insulin sensitivity by promoting expression of peroxisome proliferator activated receptor (PPAR) delta in skeletal muscle and adipose tissue. Another important action on insulin sensitivity executed by vitamin D is via narrow intracellular maintenance of calcium. Any perturbations in intracellular calcium levels in the target tissue usually results in peripheral insulin resistance. Low vitamin D induces insulin resistance via promoting hyperparathyroidism, increased (Parathyroid) PTH levels are intricately associated with diabetes. In addition, insufficient levels of vitamin D increases renin level and activate Renin-angiotensin-aldosterone (RAAS) system, subsequently angiotensin II limit the action of insulin in target organs, leading to glucose intolerance.
Vitamin D – A Regulator of Inflammatory Pathway
Accentuated inflammatory pathways have considerable importance in insulin resistance and various metabolic syndrome. Optimum level of vitamin D could directly or indirectly reduce the effects of systemic inflammation in type 2 diabetes. Studies have shown that vitamin D supplementation suppresses cytokine induced apoptosis and hence improve insulin sensitivity. NF-kB is master regulator of inflammation, as it regulates the expression of (Tumor Necrosis Factor) TNF-alpha and other proinflammatory molecules, vitamin D is known to suppress the expression of (nuclear factor kappa-light-chain-enhancer of activated B cells) NF-kB. There are strong evidence supporting this notion, monocytes isolated from type 2 diabetic patient when incubated with vitamin D suppresses the expression of cytokines such as (Interleukin) IL-6, IL-1 and TNF alpha which are known to cause insulin resistance. Additional protective effects of vitamin D supplementation include attenuation of dendritic cell differentiation, lymphocytes proliferation, foam cell formation.
Low vitamin D level is a risk factor for type 2 diabetes. Studies conducted in United Kingdom showed patients who had no diabetic history but had low vitamin D level showed high risk for hyperglycemia and insulin resistance. A cohort study conducted with 9841 subjects without diabetes over period of 29 years showed lower vitamin D level as a risk factor for type 2 diabetes. Apparently, Mendelian study analysis showed insufficient levels were not inherently associated with probability of type 2 diabetes.
Beneficial outcome of vitamin D supplementation in rescuing diabetes have produced ambiguous results. Vitamin D supplementation reduces inflammation but it has failed to show some promising results related to glycemic control. Clinical trials including sufficient sample administered with optimal dose of vitamin D, time of study periods, primary outcomes like cardiovascular disease are still warranted to further substantiate the intricate relationship between vitamin D level and onset of diabetes.


Very informative
LikeLike
Very nutritious research
LikeLike
Awesome research
LikeLike